1. Introduction (MyLive 2025)
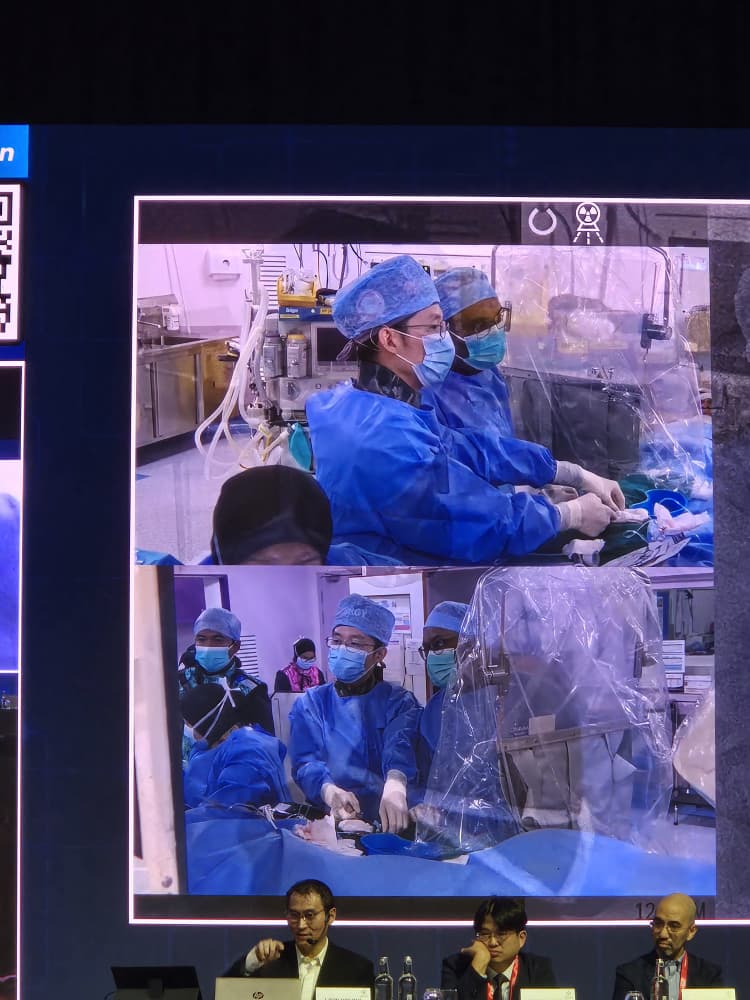
MyLive 2025: Bifurcation lesions—where a main vessel divides into two branches—remain one of the toughest challenges in percutaneous coronary intervention (PCI). When combined with heavy calcification and tortuosity, the complexity increases dramatically. The “Live-in-the-Box” session at MyLive 2025 featured an advanced hybrid strategy in one such case: a severely calcified and tortuous LAD-diagonal bifurcation, treated with rotational atherectomy (RA, also known as rota) and a tailored stenting approach.

2. Case Summary
- Patient profile: High risk, with an LAD-diagonal bifurcation lesion showing heavy calcification and tortuosity.
- Objective: Optimize luminal gains while minimizing risk to both LAD and its diagonal branch.
3. Technique & Strategy
A. Preparing the lesion—Rotational Atherectomy
- The case utilized rotablation in the LAD & diagonal to modify heavily calcified plaque. This helps facilitate stent delivery and expansion.
- Key points:
- Rotational burr selection tailored to vessel size and lesion length.
- Use of small step-downs, short ablations, pecking technique to prevent complications.
B. Hybrid Bifurcation Stenting Strategy
Instead of a standard single- or two-stent technique, the operators applied a hybrid approach. Hybrid here means combining devices and techniques from multiple established bifurcation strategies to suit lesion anatomy:
- Provisional stenting of the main vessel (LAD) with an option to “convert” to a two-stent technique if the side branch (Diagonal) was compromised.
- Use of jailing of the diagonal wire, with preparation for further treatment (kissing balloon, TAP, mini-crush, etc.), depending on side-branch quality and flow.
- Precise final optimization with proximal optimization technique (POT) to ensure good stent scaffold at the bifurcation and avoid malapposition.
4. Procedural Highlights & Nuances
- Rail-backup & guiding catheter: Adequate support was essential due to vessel tortuosity.
- Wire strategy: Dual wire setup; careful placement in both LAD and diagonal. Possibly use of anchoring or buddy wire.
- Imaging: Intravascular imaging (IVUS or OCT) likely used to assess calcium burden, vessel diameter, assess depth of burr pass, and confirm stent expansion and apposition.
- Stent selection & deployment: Drug-eluting stents sized for LAD; side-branch may have been managed with a smaller stent or balloon depending on flow. Common two-stent methods (e.g., TAP, mini-crush) used when needed.
5. Outcomes from the Live Case
- Restoration of lumen in both LAD and diagonal; excellent flow (TIMI 3) post-procedure.
- No major complications (no perforation, no severe dissection, minimal side-branch compromise).
- Optimal stent expansion confirmed, side-branch preserved.
6. Lessons Learned & Clinical Pearls
| Challenge | Approach | Key Take-home |
|---|---|---|
| Heavy calcification impeding stent passage | Use of rotational atherectomy in LAD (and diagonal if needed) | RA should be considered early in severely calcified bifurcations |
| Risk to side-branch (diagonal) during LAD stenting | Wire protection; readiness to convert to two-stent strategy | A hybrid plan allows flexibility |
| Ensuring stent scaffold geometry | Use of POT; possibly kissing balloon technique | Proper final optimization yields better long-term outcomes |
| Imaging under-utilised in many centers | Use of IVUS/OCT guides decisions on calcium modification, sizing, apposition | Imaging is not optional—it’s critical in complex anatomy |

7. Context & Implications for Practice
This case demonstrates the evolution from rigid technique selection (ergo always provisional or always two-stent) toward lesion-tailored hybrid strategies, especially in bifurcations with heavy calcium. It underscores:
- Interventionist adaptability: being ready to switch strategy mid-procedure.
- Calcium modification (rotablation, shockwave, lithotripsy) often necessary before stenting in complex lesions.
- Role of imaging and precise stent deployment techniques for procedural success and long-term vessel patency.
8. Conclusion
The “Live-in-the-Box” LAD-diagonal bifurcation case by Drs. Kumara & Lim at MyLive 2025 encapsulated the frontier of PCI: blending calcium modification with a hybrid bifurcation strategy to approach an unforgiving lesion. For interventional cardiologists, this underscores that success in complex bifurcations relies not just on technical mastery, but on procedural planning, anatomical assessment, adaptable strategy, and diligent optimization.

Met old friends from HSAJB, Dr Tee Choon Keong & Dr Sim Jian Hao!

From left Dr Lee Wei Liang, Dr David Yong (Gleneagles KL), Dr Teh Khai Chih, Dr Lim Yuen Han

With Dr Teh Khai Chih, Dr Lee Wei liang, Dr Lim Yuen Han, Chris from Edwards TAVI team, Darien Suah, Head of Division from Avelon Healthcare Group.

Dr Rhuban, Dr Ariff, Dr Faten Aqilah, Melissa from Biosensor International.
